Insurance Third Party Administrators Market Size 2025-2029
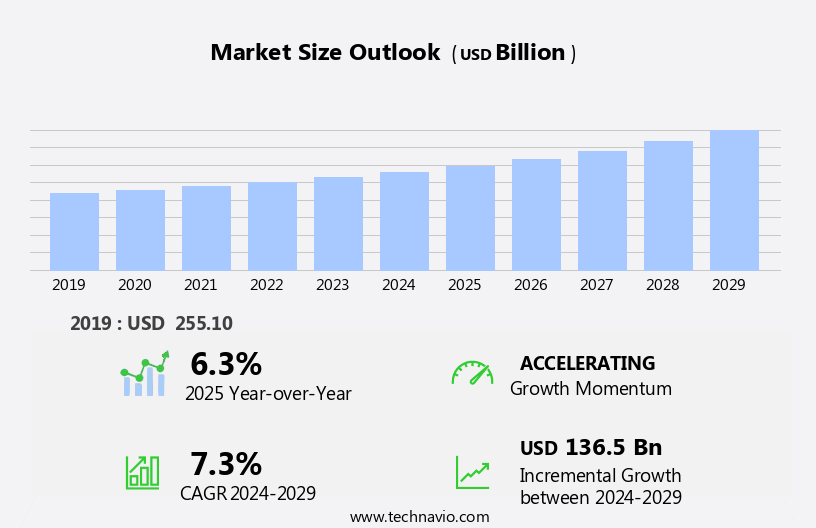
The insurance third party administrators market size is forecast to increase by USD 136.5 billion at a CAGR of 7.3% between 2024 and 2029.
- The Insurance Third Party Administrators (TPA) market experiences robust growth, driven by the increasing demand for specialized services in the insurance industry. As businesses seek to streamline operations and improve efficiency, the outsourcing of administrative functions to TPAs becomes an attractive option. Technological advancements further fuel market expansion, enabling TPAs to offer advanced services such as digital claims processing and data analytics. However, market growth is not without challenges. Regulatory hurdles impact adoption, with stringent regulations governing data privacy and security, requiring TPAs to invest significantly in compliance measures.
- Supply chain inconsistencies also temper growth potential, as TPAs rely on various stakeholders, including insurance companies, healthcare providers, and claims adjusters, to deliver services effectively. Despite these challenges, the market presents significant opportunities for companies that can navigate these complexities and provide innovative solutions to meet the evolving needs of the insurance industry.
What will be the Size of the Insurance Third Party Administrators Market during the forecast period?
- Understanding the Dynamics and Trends in the US Third-Party Administration Market The third-party administration (TPA) market in the US is experiencing significant growth and innovation, driven by the increasing demand for efficient and effective management of employee benefits and insurance programs. TPA services encompass various functions, including utilization management, performance measurement, change management, and fraud detection in life insurance, group health plans, and government programs. Customer experience is a top priority, with machine learning and predictive modeling enabling personalized services and real-time analytics. Data governance and interoperability are essential for ensuring data security and accuracy in data warehousing and API integration.
- Ethical practices and industry consortiums promote social responsibility and transparency. TPA companies invest in innovation hubs, agile development, and mobile applications to streamline policy administration and claims processing. Compliance consulting and risk modeling help organizations navigate complex regulatory requirements. Wellness programs and provider contracting are crucial components of managed care, while network management and medical billing optimize costs and improve financial reporting. Security audits, disaster recovery, business continuity, and project management ensure business resilience, while data visualization and business intelligence tools enhance customer satisfaction. Long-term care and compliance consulting further expand the scope of TPA services.
How is this Insurance Third Party Administrators Industry segmented?
The insurance third party administrators industry research report provides comprehensive data (region-wise segment analysis), with forecasts and estimates in "USD billion" for the period 2025-2029, as well as historical data from 2019-2023 for the following segments.
- Service Type
- Health plan administrators
- Workers compensation TPA
- Third party claims administration
- Type
- Large enterprises
- Small and medium enterprise
- Service
- Claims management
- Policy management
- Commission management
- Application
- Healthcare
- Construction
- Real estate
- Hospitality
- Others
- Geography
- North America
- US
- Canada
- Mexico
- Europe
- France
- Germany
- Italy
- Spain
- The Netherlands
- UK
- Middle East and Africa
- UAE
- APAC
- China
- India
- Japan
- South Korea
- South America
- Brazil
- Rest of World (ROW)
- North America
By Service Type Insights
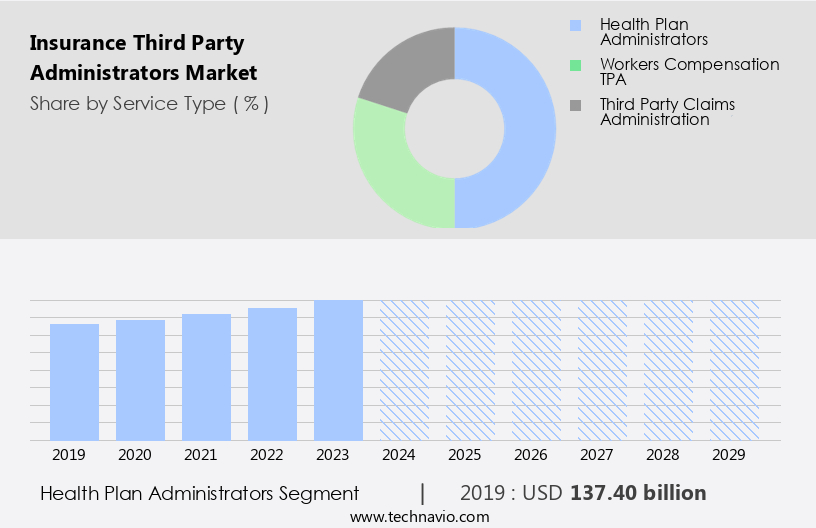
The health plan administrators segment is estimated to witness significant growth during the forecast period.
Health plan administrators, including those serving Large Enterprise Insurance and Health Insurance, play a pivotal role in the healthcare ecosystem by managing various administrative tasks related to health insurance plans on behalf of employers, insurance companies, or self-insured organizations. Their primary responsibilities include claim processing, enrollment and eligibility management, and premium billing and management. The integration of technology is significantly impacting the operations of health plan administrators. For instance, Cloud Computing facilitates data accessibility and storage, enabling real-time data processing and analysis. Data Security ensures the confidentiality and integrity of sensitive health information. Digital Transformation, including Workflow Automation and Process Efficiency, streamlines administrative tasks and reduces manual labor, leading to Cost Optimization.
Compliance Services ensure adherence to regulatory requirements, while Data Analytics and Data Privacy provide valuable insights and protect member data. Blockchain Technology enhances transparency and security in claims processing and fraud detection. Machine Learning and Predictive Analytics enable Risk Assessment and Personalized Services, improving customer experience. Healthcare Providers, Insurance Carriers, and Government Programs are key stakeholders in the health insurance ecosystem. Strategic Partnerships and Technology Integration enable seamless communication and data exchange between these entities. Workers' Compensation, Disability Insurance, Individual Health Plans, and Group Health Plans all require efficient claims administration and automated claims processing. Underwriting Support and Risk Management ensure accurate risk assessment and cost containment for Self-Funded Plans.
Virtual Assistants and Artificial Intelligence provide efficient member services, including Enrollment Processing and Benefits Management. Outsourcing Services offer cost savings and expertise in specialized areas, such as Compliance and Data Governance. In conclusion, health plan administrators are essential players in the health insurance industry, providing critical services that ensure the efficient operation of health insurance plans.
The Health plan administrators segment was valued at USD 137.40 billion in 2019 and showed a gradual increase during the forecast period.
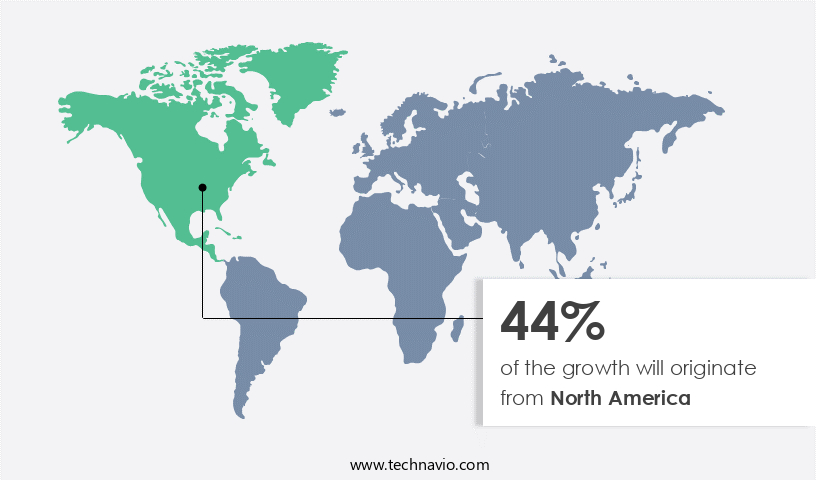
Regional Analysis
North America is estimated to contribute 44% to the growth of the global market during the forecast period.Technavio's analysts have elaborately explained the regional trends and drivers that shape the market during the forecast period.
The Insurance Third Party Administrators (TPA) market in North America is experiencing significant growth due to the region's thriving insurance industry, diverse product offerings, and regulatory environment. Insurance companies in North America are increasingly outsourcing administrative functions to TPAs to streamline operations, reduce costs, and focus on core competencies. Outsourcing tasks such as claims processing, policy administration, and customer service enables insurers to improve efficiency and scalability. Digital transformation is a key trend in the market, with the adoption of cloud computing, workflow automation, and artificial intelligence driving process efficiency and risk assessment. Compliance services and data security are also critical areas of focus for TPAs, ensuring data privacy and governance for individual health plans, group health plans, self-funded plans, and workers' compensation.
TPAs are also leveraging predictive analytics and machine learning to enhance underwriting support, risk management, and fraud detection. Strategic partnerships with insurance carriers, healthcare providers, and government programs are further expanding the market's reach and scope. Cost optimization is a significant factor, with TPAs offering cost containment solutions for insurers. Automated claims processing and benefits management are also essential services, improving customer experience and streamlining enrollment processing and technology integration. Blockchain technology is an emerging trend, offering potential for increased transparency and security in the insurance industry. Virtual assistants and digital health are also transforming the market, offering personalized services and enabling real-time risk assessment and claims processing.
In summary, the market in North America is growing due to the increasing demand for administrative outsourcing services, digital transformation, cost optimization, and regulatory compliance. TPAs are offering a range of services, from claims processing and policy administration to risk assessment and fraud detection, enabling insurers to focus on their core competencies while improving efficiency, reducing costs, and enhancing customer experiences.
Market Dynamics
Our researchers analyzed the data with 2024 as the base year, along with the key drivers, trends, and challenges. A holistic analysis of drivers will help companies refine their marketing strategies to gain a competitive advantage.
What are the Insurance Third Party Administrators market drivers leading to the rise in the adoption of Industry?
- The surge in demand for specialized insurance services is the primary market driver in the insurance industry.
- Insurance Third Party Administrators (TPAs) provide essential services to insurers and small businesses in managing their insurance programs. TPAs specialize in claims management, processing enrollment, offering member services, benefits management for self-funded plans, and underwriting support. They efficiently handle the entire claims process, from receiving claims to thorough evaluation, investigation, and settlement, ensuring compliance with policy terms and regulations. TPAs utilize data analytics to identify trends and patterns, enabling cost containment and effective claim management. TPAs prioritize data privacy and security, ensuring sensitive information is protected. They integrate technology to streamline processes, such as automating enrollment and claims processing.
- TPAs also offer customer service and support, including policyholder inquiries and claims status updates. Risk management services include risk assessment, safety recommendations, and implementing loss control programs to prevent insured events and reduce claims. TPAs negotiate with healthcare providers to manage claim costs effectively and ensure proper settlements. Fraudulent claims are identified and prevented through rigorous verification processes, safeguarding insurers from financial losses.
What are the Insurance Third Party Administrators market trends shaping the Industry?
- The trend in the insurance industry is being shaped by technological advancements in Third-Party Administrators (TPAs). This includes the implementation of automation, artificial intelligence, and data analytics to streamline processes and enhance efficiency. Technological innovations are increasingly becoming mandatory for insurance TPAs to remain competitive and provide superior services to clients.
- Insurance Third Party Administrators (TPAs) are leveraging advanced technologies, including artificial intelligence (AI) and robotic process automation (RPA), to optimize their services and enhance the customer experience. RPA software robots automate repetitive tasks such as data entry, document processing, and claims validation, reducing errors, increasing throughput, and freeing up human resources for more complex tasks. AI and machine learning (ML) technologies enable TPAs to analyze large datasets, extract valuable insights, and make data-driven decisions. This transformation of insurance TPA operations leads to improved efficiency, accuracy, and personalized services for various sectors, including life insurance, group health plans, and government programs.
- Furthermore, the integration of AI and ML technologies in fraud detection systems bolsters the industry's efforts to combat fraudulent activities and maintain trust with healthcare providers and policyholders. Data governance practices ensure the security and privacy of sensitive information throughout the process, further strengthening the TPAs' commitment to delivering high-quality services.
How does Insurance Third Party Administrators market faces challenges face during its growth?
- The lack of industry awareness regarding the roles and functions of insurance Third-Party Administrators (TPAs) represents a significant challenge impeding the growth of the insurance sector.
- The insurance third party administrators (TPA) market faces growth challenges due to insufficient awareness and understanding of these services in certain regions, particularly in emerging markets. This lack of awareness hinders the expansion of the TPAs' client base and limits their reach to potential customers. Consequently, insurers, brokers, and self-insured entities may overlook the benefits of outsourcing administrative functions to TPAs. Digital transformation, including the adoption of blockchain technology, workflow automation, and cloud computing, is driving innovation in the insurance industry. TPAs are well-positioned to provide compliance services and cost optimization solutions in this digital landscape. However, data security concerns remain a significant challenge.
- In the health insurance sector, digital health solutions are gaining traction. TPAs can leverage these trends to offer value-added services and enhance their offerings. Workers' compensation is another area where TPAs can provide expertise and efficiency. By addressing these opportunities and overcoming awareness hurdles, insurance TPAs can strengthen their market position and contribute to the digital transformation of the insurance industry.
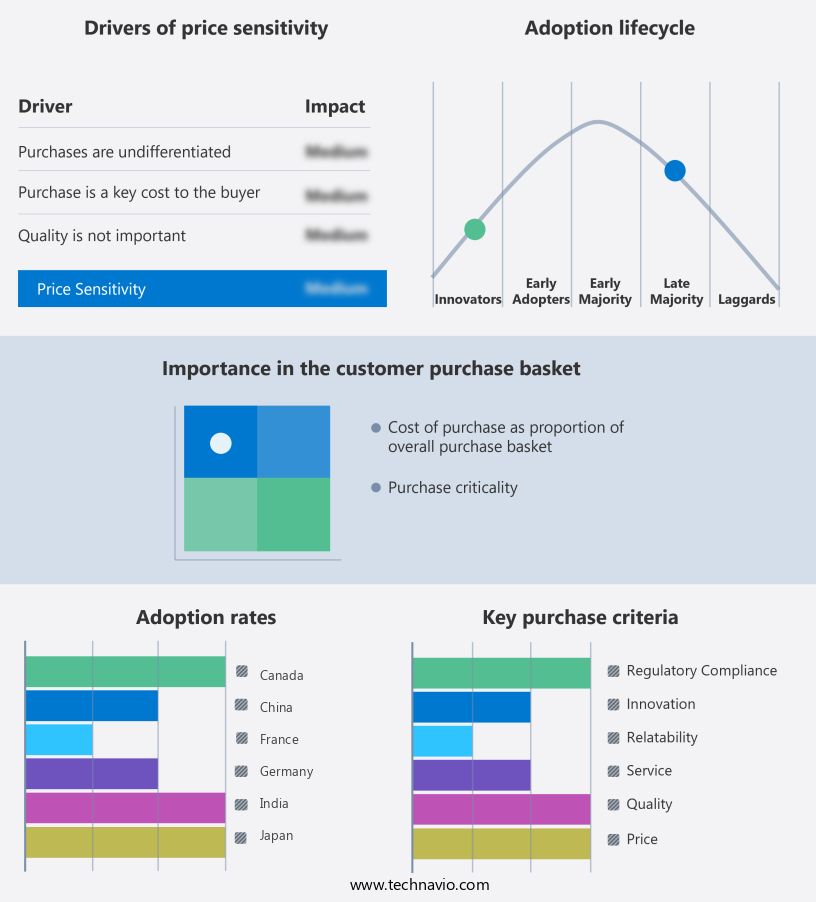
Exclusive Customer Landscape
The insurance third party administrators market forecasting report includes the adoption lifecycle of the market, covering from the innovator's stage to the laggard's stage. It focuses on adoption rates in different regions based on penetration. Furthermore, the insurance third party administrators market report also includes key purchase criteria and drivers of price sensitivity to help companies evaluate and develop their market growth analysis strategies.
Customer Landscape
Key Companies & Market Insights
Companies are implementing various strategies, such as strategic alliances, insurance third party administrators market forecast, partnerships, mergers and acquisitions, geographical expansion, and product/service launches, to enhance their presence in the industry.
The industry research and growth report includes detailed analyses of the competitive landscape of the market and information about key companies, including:
- Accenture Japan Ltd. (Japan, operations)
- Allianz Global Assistance (Germany)
- Broadspire (United States)
- Capita plc (United Kingdom)
- CorVel Corporation (United States)
- Crawford & Company (United States)
- DXC Technology (United States, operations)
- Gallagher Bassett Services Inc. (United States)
- Generali Global Assistance (France)
- HCL Technologies Ltd. (India)
- Helmsman Management Services (United States)
- Infosys Ltd. (India)
- Munich Re Digital Partners (Germany)
- NTT Data Corporation (Japan)
- Samsung Fire & Marine Insurance (South Korea)
- Sedgwick Claims Management Services Inc. (United States)
- Tata Consultancy Services Ltd. (India)
- UMR Inc. (United States)
- Wipro Ltd. (India)
- York Risk Services Group (United States)
Qualitative and quantitative analysis of companies has been conducted to help clients understand the wider business environment as well as the strengths and weaknesses of key industry players. Data is qualitatively analyzed to categorize companies as pure play, category-focused, industry-focused, and diversified; it is quantitatively analyzed to categorize companies as dominant, leading, strong, tentative, and weak.
Recent Development and News in Insurance Third Party Administrators Market
- In February 2024, Willis Towers Watson, a leading global advisory, broking, and solutions company, announced the launch of its new digital third-party administration (TPA) platform, "WTW TPA Connect." This innovative solution aims to streamline claims processing and improve operational efficiency for insurers and self-insured organizations (Willis Towers Watson Press Release, 2024).
- In October 2025, Cigna Corporation, a major health services company, entered into a strategic partnership with Change Healthcare, a healthcare technology firm, to enhance their TPA capabilities. The collaboration focuses on implementing Change Healthcare's Intelligent Healthcare Network to process claims more effectively and efficiently, improving the overall customer experience (Cigna Press Release, 2025).
- In March 2024, Marsh McLennan Companies, a global professional services firm, completed the acquisition of Jardine Lloyd Thompson Group plc, a leading TPA and insurance brokerage firm. This acquisition significantly expanded Marsh McLennan's global reach and capabilities in the TPA market, positioning them as a major player (Marsh McLennan Companies Press Release, 2024).
- In July 2025, the National Association of Insurance Commissioners (NAIC) approved new regulations for TPAs, requiring them to maintain minimum capital and liquidity requirements. This initiative aims to ensure TPAs' financial stability and protect policyholders, enhancing the overall market's integrity (NAIC Press Release, 2025).
Research Analyst Overview
The insurance third-party administrators (TPA) market continues to experience dynamic shifts as large enterprises seek innovative solutions to manage their health insurance programs. TPA services encompass a broad range of functions, from compliance services and workflow automation to cost optimization and risk assessment. Blockchain technology is increasingly being explored in the insurance industry as a means to enhance data security and streamline processes. TPAs are integrating this technology to ensure secure and transparent data exchange between stakeholders, ultimately improving process efficiency and reducing the risk of fraud. Digital transformation is another key trend in the TPA market, with the adoption of cloud computing and automation playing a significant role.
Digital health and virtual assistants powered by artificial intelligence (AI) are transforming the way TPAs manage claims administration and member services. Cost optimization remains a critical priority for TPAs, with data analytics and data privacy playing essential roles. TPAs are leveraging data analytics to gain insights into risk assessment, predictive analytics, and cost containment. Data privacy is also a major concern, with TPAs implementing robust data governance practices to protect sensitive information. TPAs are also focusing on process efficiency and risk management, with strategic partnerships and technology integration being key areas of investment. Insurance carriers are increasingly collaborating with TPAs to provide personalized services and improve the customer experience.
Small business insurance is another growing segment in the TPA market, with TPAs offering outsourcing services to help small businesses manage their insurance programs. Self-funded plans and cost containment are major concerns for small businesses, and TPAs are providing underwriting support and claims processing services to help them manage these risks. Risk assessment and fraud detection are critical functions for TPAs, with machine learning and predictive analytics being used to identify potential risks and prevent fraudulent claims. TPAs are also collaborating with healthcare providers and government programs to improve the accuracy of risk assessments and reduce the administrative burden on healthcare providers.
In the realm of life insurance, TPAs are leveraging technology to streamline policy administration and improve the customer experience. Disability insurance and individual health plans are other areas where TPAs are providing value-added services, from enrollment processing to benefits management. In conclusion, the TPA market is undergoing significant changes as large enterprises and small businesses seek innovative solutions to manage their insurance programs. TPAs are leveraging technology, data analytics, and strategic partnerships to improve process efficiency, reduce costs, and enhance the customer experience. Blockchain technology, digital health, and risk assessment are some of the key areas of investment, with a focus on data security, cost optimization, and risk management.
Dive into Technavio's robust research methodology, blending expert interviews, extensive data synthesis, and validated models for unparalleled Insurance Third Party Administrators Market insights. See full methodology.
|
Market Scope |
|
|
Report Coverage |
Details |
|
Page number |
240 |
|
Base year |
2024 |
|
Historic period |
2019-2023 |
|
Forecast period |
2025-2029 |
|
Growth momentum & CAGR |
Accelerate at a CAGR of 7.3% |
|
Market growth 2025-2029 |
USD 136.5 billion |
|
Market structure |
Fragmented |
|
YoY growth 2024-2025(%) |
6.3 |
|
Key countries |
US, China, Japan, Germany, France, Spain, Canada, India, South Korea, France, Japan, Italy, Brazil, UAE, UK, Spain, Rest of World (ROW), Mexico, and The Netherlands |
|
Competitive landscape |
Leading Companies, Market Positioning of Companies, Competitive Strategies, and Industry Risks |
What are the Key Data Covered in this Insurance Third Party Administrators Market Research and Growth Report?
- CAGR of the Insurance Third Party Administrators industry during the forecast period
- Detailed information on factors that will drive the growth and forecasting between 2025 and 2029
- Precise estimation of the size of the market and its contribution of the industry in focus to the parent market
- Accurate predictions about upcoming growth and trends and changes in consumer behaviour
- Growth of the market across North America, APAC, Europe, Middle East and Africa, and South America
- Thorough analysis of the market's competitive landscape and detailed information about companies
- Comprehensive analysis of factors that will challenge the insurance third party administrators market growth of industry companies
We can help! Our analysts can customize this insurance third party administrators market research report to meet your requirements.