Healthcare Payer Network Management Market Size 2026-2030
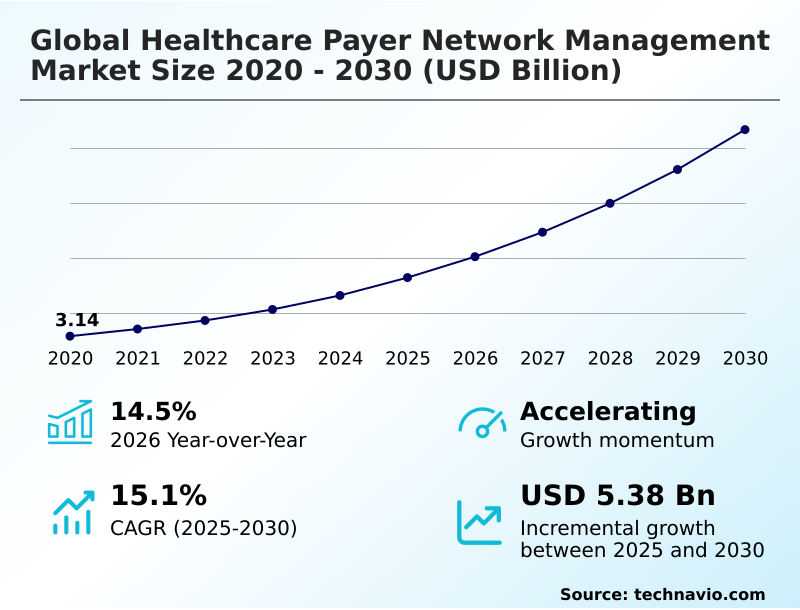
The healthcare payer network management market size is valued to increase by USD 5.38 billion, at a CAGR of 15.1% from 2025 to 2030. Adoption of AI for cost containment and fraud prevention will drive the healthcare payer network management market.
Major Market Trends & Insights
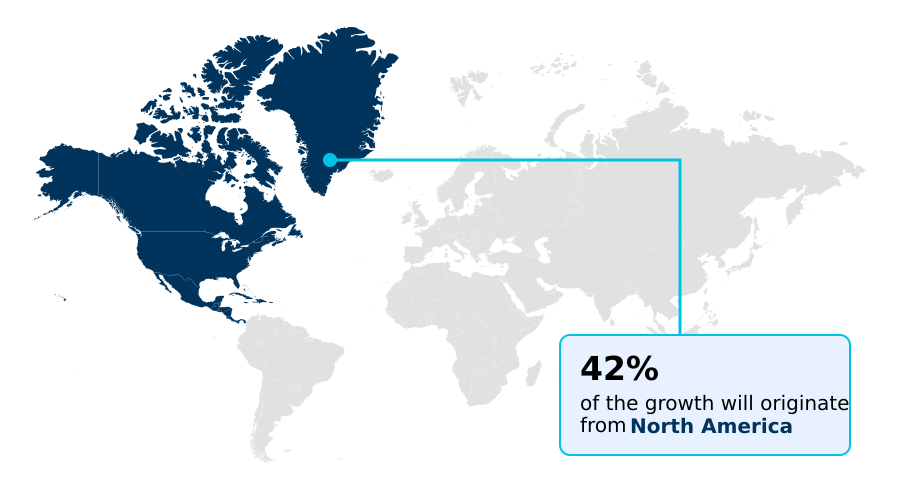
- North America dominated the market and accounted for a 41.6% growth during the forecast period.
- By Component - Platform and software segment was valued at USD 2.89 billion in 2024
- By Delivery Mode - Cloud segment accounted for the largest market revenue share in 2024
Market Size & Forecast
- Market Opportunities: USD 7.51 billion
- Market Future Opportunities: USD 5.38 billion
- CAGR from 2025 to 2030 : 15.1%
Market Summary
- The healthcare payer network management market is undergoing a significant transformation, driven by the dual pressures of cost containment and the industry-wide shift to value-based care models. Payers are increasingly adopting advanced software and platforms to automate historically manual processes, such as provider data management and claims adjudication, to enhance operational efficiency.
- This technological shift is critical for managing complex provider relationships and ensuring regulatory adherence. For instance, a private insurer can leverage a unified platform for provider onboarding, integrating data from various sources to accelerate credentialing and contracting, which directly improves network adequacy and member satisfaction.
- Key trends include the integration of AI for predictive analytics, the development of consumer-facing transparency tools, and the expansion of virtual care networks. However, challenges persist, including the integration of modern solutions with legacy IT systems, the constant threat of cybersecurity breaches, and the complexities of maintaining accurate provider directories to comply with regulations like the No Surprises Act.
- This dynamic environment necessitates continuous investment in technology to balance cost, quality, and member access.
What will be the Size of the Healthcare Payer Network Management Market during the forecast period?
Get Key Insights on Market Forecast (PDF) Request Free Sample
How is the Healthcare Payer Network Management Market Segmented?
The healthcare payer network management industry research report provides comprehensive data (region-wise segment analysis), with forecasts and estimates in "USD million" for the period 2026-2030, as well as historical data from 2020-2024 for the following segments.
- Component
- Platform and software
- Services
- Delivery mode
- Cloud
- On-premises
- End-user
- Public health insurance
- Private health insurance
- Geography
- North America
- US
- Canada
- Mexico
- Europe
- Germany
- UK
- France
- Asia
- Rest of World (ROW)
- North America
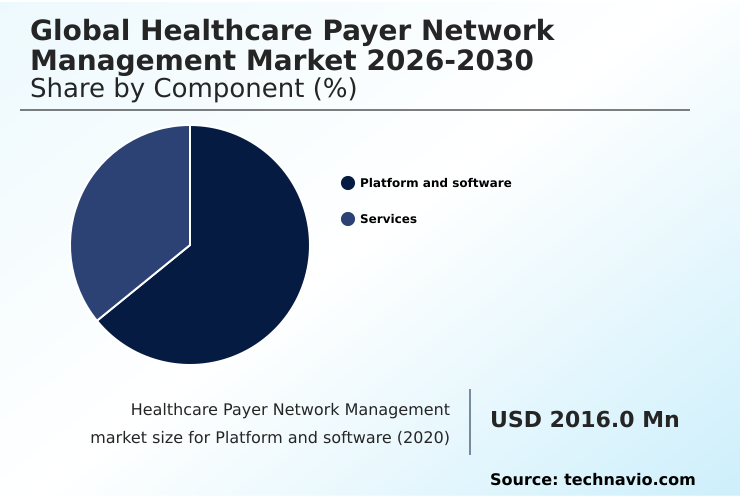
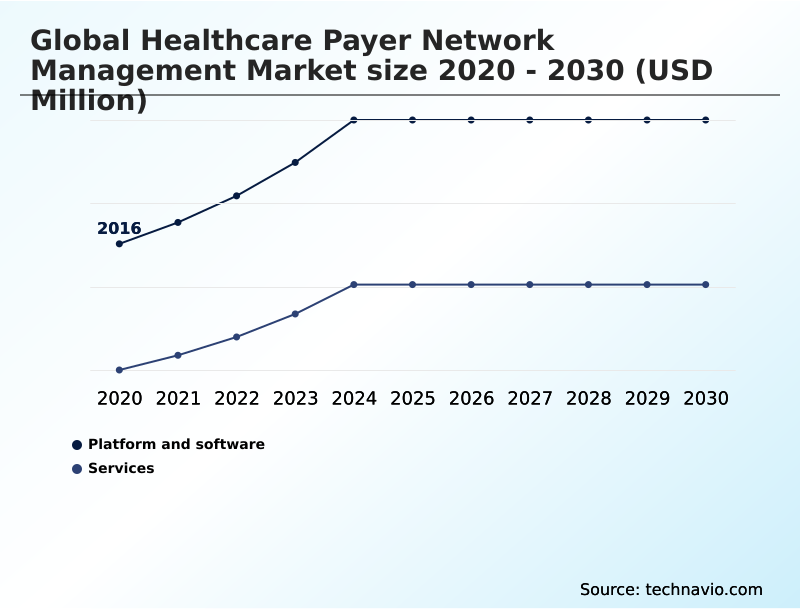
By Component Insights
The platform and software segment is estimated to witness significant growth during the forecast period.
The platform and software segment is central to healthcare payer operations, enabling efficient network administration through advanced technological solutions. Payers are deploying sophisticated software to move beyond manual workflows, adopting tools for provider credentialing automation and detailed network adequacy analysis.
These systems are essential for managing the complexities of value-based care reimbursement and ensuring regulatory compliance reporting. Core administrative systems are being upgraded with modules for real-time claims processing and contract lifecycle management, which includes fee schedule management.
A key business driver is operational efficiency, with some payers achieving a 40% reduction in provider onboarding time by implementing AI-driven digital credentialing workflows. This focus on automation helps ensure provider directory accuracy and strengthens payer-provider collaboration tools.
The Platform and software segment was valued at USD 2.89 billion in 2024 and showed a gradual increase during the forecast period.
Regional Analysis
North America is estimated to contribute 41.6% to the growth of the global market during the forecast period.Technavio’s analysts have elaborately explained the regional trends and drivers that shape the market during the forecast period.
See How Healthcare Payer Network Management Market Demand is Rising in North America Request Free Sample
The healthcare payer network management market exhibits distinct regional dynamics, with North America accounting for over 41% of the incremental growth, driven by stringent regulations and the transition to value-based care.
In this region, payers focus on provider network optimization and predictive network analytics. Europe emphasizes cross-border health data exchange and compliance with data privacy laws, using payment integrity solutions to manage costs.
The market in Asia is characterized by rapid technology adoption, particularly mobile health application support and telehealth provider integration to bridge access gaps. Payers in this region are implementing provider performance scorecards and population health management analytics to improve outcomes.
This global divergence in priorities highlights the need for adaptable solutions that can handle both mature, regulation-heavy markets and high-growth regions focused on digital-first strategies.
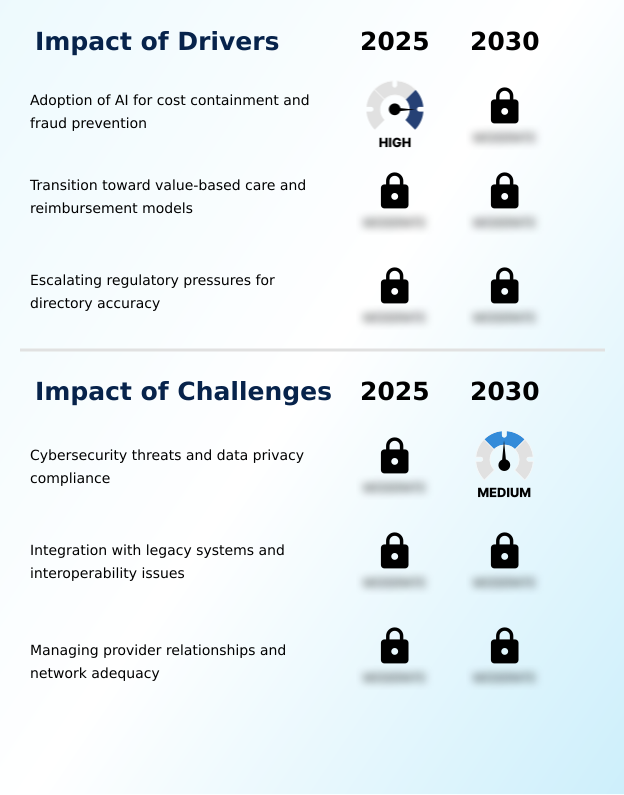
Market Dynamics
Our researchers analyzed the data with 2025 as the base year, along with the key drivers, trends, and challenges. A holistic analysis of drivers will help companies refine their marketing strategies to gain a competitive advantage.
- The global healthcare payer network management market is evolving to address highly specific operational and strategic challenges. Insurers are increasingly focused on improving provider directory accuracy to meet regulatory demands and enhance member experience. For government-sponsored programs, managing provider networks for medicaid requires specialized platforms that can handle complex compliance and reporting needs.
- The adoption of AI for provider credentialing verification is becoming standard, significantly reducing manual effort. Similarly, advanced analytics for high-performance network design allow payers to construct networks that balance cost and quality effectively. As the industry moves toward more complex reimbursement structures, software for value-based contract modeling and technology for value-based reimbursement are critical.
- Integrating telehealth provider networks into existing frameworks is another key focus, demanding new approaches to credentialing and quality monitoring. Payers are also deploying sophisticated tools for no surprises act compliance and solutions for provider data synchronization to prevent surprise billing with accurate data.
- These targeted solutions, such as those for managing risk-sharing agreements with providers and technology for cross-border health insurance, are delivering measurable returns, with some platforms reducing claims processing errors by a greater margin than legacy systems. This specialization extends to automating provider contract lifecycle management, using platforms for real-time claims adjudication, and building a consumer-centric provider directory.
- Furthermore, payers are exploring how to integrate social determinants into networks and are using specialized fraud detection in payer provider networks to protect revenue.
What are the key market drivers leading to the rise in the adoption of Healthcare Payer Network Management Industry?
- The adoption of AI for cost containment and fraud prevention serves as a key driver, enabling payers to reduce administrative overhead and protect revenue integrity.
- Market growth is primarily fueled by the need for operational efficiency and regulatory adherence. The adoption of value-based care models necessitates robust solutions for managing reimbursement incentive calculation and supporting care management program integration.
- These platforms enable payers to execute complex risk-sharing agreement management, which can improve cost predictability by 15%. Escalating regulatory pressures for directory accuracy are driving investment in automated provider directory synchronization and ghost network identification technologies.
- The use of provider data verification tools and automated provider onboarding systems streamlines administrative tasks, reducing manual errors by over 40% in some cases.
- This focus on automation not only ensures compliance but also enhances the ability to manage intricate managed care contract negotiation and supports a broader population health management support strategy.
What are the market trends shaping the Healthcare Payer Network Management Industry?
- The integration of machine learning is a transformative trend, enabling advanced network optimization and predictive analytics for payers. This shift allows for more dynamic and data-driven management of provider networks to improve efficiency and care quality.
- Key trends are reshaping the healthcare payer network management landscape, driven by technology and consumer demands. The adoption of virtual-first care models and hybrid provider networks is accelerating, requiring sophisticated specialist referral management and remote monitoring reimbursement frameworks. This shift is supported by consumer-centric digital platforms that incorporate price transparency tools and automated outreach tools, improving member experience.
- These platforms can increase user satisfaction by up to 25%. Internally, payers are leveraging machine learning for network performance monitoring and claims repricing engine optimization. The focus on claims dispute resolution portals and quality metric reconciliation supports a more collaborative clinical governance framework, where data-driven insights enhance partnerships between payers and providers.
- This evolution toward a digital, transparent, and integrated ecosystem is now a market standard.
What challenges does the Healthcare Payer Network Management Industry face during its growth?
- Significant challenges related to cybersecurity threats and data privacy compliance affect industry growth, requiring substantial investment in security protocols and adherence to complex regulations.
- The market faces significant challenges that can impede progress and increase operational costs. Cybersecurity and compliance with data privacy regulations are paramount, demanding secure platforms for credentialing lifecycle management and patient referral tracking. The integration of modern software with legacy systems creates interoperability bottlenecks, hindering efforts to achieve seamless data exchange and real-time updates.
- This technical debt makes it difficult to implement functionalities like provider performance scorecards or to incorporate social determinants of health data effectively. Managing provider relationships is also complex, with payers needing to balance network gap analysis with contract negotiations. Failure to maintain adequate networks can lead to regulatory penalties that are 20% higher than in previous years.
- These hurdles require strategic investments in both technology modernization and partnership management to ensure sustainable growth.
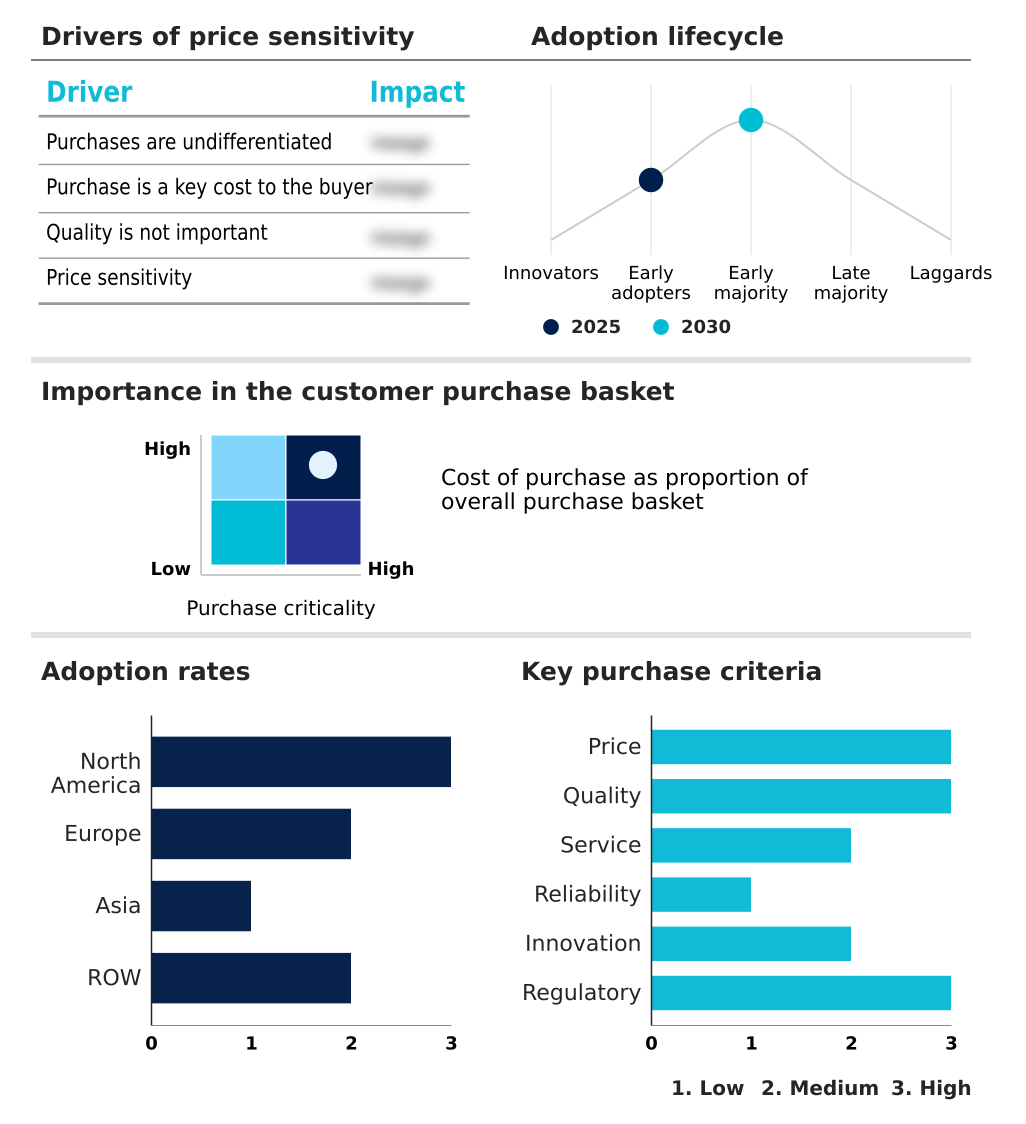
Exclusive Technavio Analysis on Customer Landscape
The healthcare payer network management market forecasting report includes the adoption lifecycle of the market, covering from the innovator’s stage to the laggard’s stage. It focuses on adoption rates in different regions based on penetration. Furthermore, the healthcare payer network management market report also includes key purchase criteria and drivers of price sensitivity to help companies evaluate and develop their market growth analysis strategies.
Customer Landscape of Healthcare Payer Network Management Industry
Competitive Landscape
Companies are implementing various strategies, such as strategic alliances, healthcare payer network management market forecast, partnerships, mergers and acquisitions, geographical expansion, and product/service launches, to enhance their presence in the industry.
Availity - Provider data management platforms streamline credentialing, directory maintenance, and information exchange, optimizing the connection between payers and providers for enhanced network integrity.
The industry research and growth report includes detailed analyses of the competitive landscape of the market and information about key companies, including:
- Availity
- Cedar Gate Technologies
- Cognizant Technology Solution
- Cotiviti Inc.
- Gainwell Technologies LLC
- HealthEdge Software Inc.
- Infosys Ltd.
- Innovaccer Inc.
- LexisNexis Risk Solutions.
- Mphasis Ltd.
- Optum Inc.
- Oracle Corp.
- Quest Analytics LLC
- Salesforce Inc.
- SS and C Technologies Inc.
- Symplr
- Verisys
- Zelis
Qualitative and quantitative analysis of companies has been conducted to help clients understand the wider business environment as well as the strengths and weaknesses of key industry players. Data is qualitatively analyzed to categorize companies as pure play, category-focused, industry-focused, and diversified; it is quantitatively analyzed to categorize companies as dominant, leading, strong, tentative, and weak.
Recent Development and News in Healthcare payer network management market
- In February 2025, Centene Corporation integrated a proprietary generative AI module into its provider network operations, designed to automate the verification of provider credentials and reduce onboarding time.
- In March 2025, UnitedHealth Group announced a strategic expansion of its outcome-based contract framework, utilizing a new proprietary analytics engine to manage risk-sharing agreements with major hospital systems.
- In April 2025, the Centers for Medicare and Medicaid Services released updated interoperability mandates requiring Medicare Advantage plans to use digital interfaces for real-time exchange of quality performance data.
- In February 2025, Humana Inc. announced a major restructuring of its specialist network contracts to prioritize value-based outcomes over volume, leading to renegotiations with several large provider groups.
Dive into Technavio’s robust research methodology, blending expert interviews, extensive data synthesis, and validated models for unparalleled Healthcare Payer Network Management Market insights. See full methodology.
| Market Scope | |
|---|---|
| Page number | 281 |
| Base year | 2025 |
| Historic period | 2020-2024 |
| Forecast period | 2026-2030 |
| Growth momentum & CAGR | Accelerate at a CAGR of 15.1% |
| Market growth 2026-2030 | USD 5378.3 million |
| Market structure | Fragmented |
| YoY growth 2025-2026(%) | 14.5% |
| Key countries | US, Canada, Mexico, Germany, UK, France, The Netherlands, Italy, Spain, Russia, China, Japan, India, South Korea, Indonesia, Thailand, Singapore, Australia, Brazil, UAE, Saudi Arabia, South Africa and Turkey |
| Competitive landscape | Leading Companies, Market Positioning of Companies, Competitive Strategies, and Industry Risks |
Research Analyst Overview
- The healthcare payer network management market is defined by a strategic imperative to modernize core administrative systems and embrace data-driven decision-making. Payers are actively implementing provider data management solutions for provider onboarding platforms and claims adjudication software to streamline operations.
- The integration of a provider relationship management crm and a robust data activation platform is critical for achieving a holistic view of network performance. Technologies for provider credentialing automation and automated provider verification are no longer optional but essential for maintaining regulatory compliance reporting and provider directory accuracy.
- Boardroom decisions are increasingly focused on investing in high-performance network design and predictive network analytics to manage costs associated with bundled payment administration and capitation payment models. This involves leveraging payment integrity solutions and fraud, waste, and abuse detection tools.
- Payers are using platforms with real-time claims processing capabilities and quality performance tracking, with some achieving a 30% reduction in provider data errors. The adoption of healthcare interoperability standards and api-driven data exchange is pivotal for enabling effective payer-provider collaboration tools.
What are the Key Data Covered in this Healthcare Payer Network Management Market Research and Growth Report?
-
What is the expected growth of the Healthcare Payer Network Management Market between 2026 and 2030?
-
USD 5.38 billion, at a CAGR of 15.1%
-
-
What segmentation does the market report cover?
-
The report is segmented by Component (Platform and software, and Services), Delivery Mode (Cloud, and On-premises), End-user (Public health insurance, and Private health insurance) and Geography (North America, Europe, Asia, Rest of World (ROW))
-
-
Which regions are analyzed in the report?
-
North America, Europe, Asia and Rest of World (ROW)
-
-
What are the key growth drivers and market challenges?
-
Adoption of AI for cost containment and fraud prevention, Cybersecurity threats and data privacy compliance
-
-
Who are the major players in the Healthcare Payer Network Management Market?
-
Availity, Cedar Gate Technologies, Cognizant Technology Solution, Cotiviti Inc., Gainwell Technologies LLC, HealthEdge Software Inc., Infosys Ltd., Innovaccer Inc., LexisNexis Risk Solutions., Mphasis Ltd., Optum Inc., Oracle Corp., Quest Analytics LLC, Salesforce Inc., SS and C Technologies Inc., Symplr, Verisys and Zelis
-
Market Research Insights
- The market is shaped by the push for greater efficiency and transparency, compelling payers to adopt modern solutions for provider network configuration and value-based contract modeling. The use of consumer-centric digital platforms is rising, with implementations showing a 30% improvement in member engagement by providing better healthcare price transparency.
- Effective out-of-network claims management and real-time eligibility verification are now standard expectations, reducing administrative friction. Adherence to interoperability standards and automated prior authorization can reduce claims denial rates by over 15%.
- This focus on technology-driven processes helps payers achieve cost of care reduction while improving both member access to care and the overall provider relationship, creating a more streamlined healthcare ecosystem.
We can help! Our analysts can customize this healthcare payer network management market research report to meet your requirements.